By Mikkel Munksgaard
Demographic megatrends, such as ageing populations, challenges public health budgets in developed countries. Currently, health costs in OECD countries are growing at roughly double the rate as the average growth in GPD. ‘Pay for Success’ is an emergent, and highly innovative, partnership model promising both increased cost-effectiveness and patient-centric services in healthcare. Whether or not the model will constitute a critical feature of future health systems, only time will tell.
Due to critical leaps in modern healthcare and medicine, the average life expectancy in developed countries has doubled since 1900 [1]. While this is an important success, it also challenges public health systems because chronic diseases occur much more often at old age. In fact, a Danish report states that the average health costs for an 86-year-old are 16 times higher than for a 20-year-old [2].
In addition, public health sectors are experiencing structural challenges inhibiting their capacity to deliver services effectively.
The lack of systematic assessments towards quality and outcomes of services creates disproportionality on financial priorities. Evidence indicates that up to 30% of healthcare expenses are wasted on unproven or unnecessary treatments.
World Economic Forum 2017
An example of this is the general de-prioritization of preventive health interventions over short-term illness treatment.
Introducing ‘Pay for Success’
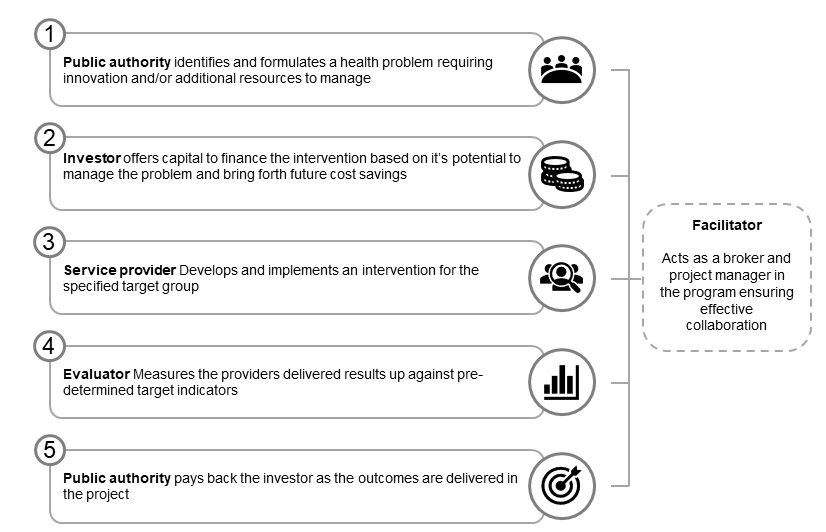
‘Pay for Success’ (PFS) has emerged as an organizational solution to the problems of asymmetry and ineffectiveness in public health. A PFS-program is fundamentally a public commissioning model based on two distinctive features 1) an outcome-based contract and 2) the engagement of an external ‘investor’.
In an outcome-based contract service delivery is outsourced to a provider and the public commissioner pays for the realization of long-term health outcomes. Hence, the public “pays for success”. Because services, such as preventive interventions, could take several years to deliver the PFS-model involves an ‘investor’ that provides working capital for the provider – and thus, takes the majority of the financial risk. This could either be a non-profit organization, a for-profit organization, or both. The first PFS-program was developed in 2010 and since then 200 programs have been initiated mobilizing a total capital of 420 Million Dollar [3]. Especially in the UK, the PFS-market has grown and is predicted to soon reach a total value of 1 Billion Euro (Carter 2019).
Challenges and future directions of ‘Pay for Success’
While empirical studies from the UK and US does indicate that the PFS-model performs better than other commissioning models [4], they also highlight a more complex organizational structure that takes time and resources to develop – which, consequently, creates high transaction costs ultimately challenging the model’s cost-effectiveness. Technical problems related to valuating health outcomes, and creating a payment structure around such, has proven difficult and time-consuming. Additionally, the complex governance structure of PFS-programs in the UK and US has been criticized for being too rigid and focused on short-term performance – thus, inhibiting innovation.
The emergence of PFS-programs in Scandinavian countries poses an interesting field as emerging research indicates that these programs are fundamentally different from traditional PFS-models. The tendency to utilize more networked practices as well as the existence of comprehensive public data systems in Scandinavian welfare states could potentially solve some of the most critical challenges currently faced in PFS-development. What would seem critical for future PFS-development is to leverage these emerging insights and shine more light into the ‘black box’ of PFS-development.
References
[2] Kjellberg and Højgaard 2017
[3] The Brookings Institution 2021
About the Author
Mikkel Munksgaard Andersen is Ph.D. Fellow at CBS, MSC. Through his Ph.D.-project, Mikkel studies the development and implementation of social impact bonds and payment-by-results methods in Denmark. His work centralizes around the distinct characteristics of Scandinavian impact bonds and their role in supporting and financing public services. The research takes a point of departure in the Danish research- and innovation project PreCare which seeks to develop new services and organizational models for preventive and digitalized healthcare. See more here.
